4 Ways To Provide Meaningful Healthcare

Recently, I was asked to share insights about Patient Experience (PX) in hospital or hospice environments. What I’m sharing is a reflection of my work in very conventional American healthcare settings, where service-minded philosophies are often known, and under-prioritized for a variety of reasons. I don’t imagine my comments will surprise anyone.
So we’re on the same page, PX explores how an organization’s culture and people influence patient perception about service, quality and care. I’m fascinated by the symbiosis generated between individuals, groups and environments. You’ll find my comments apply to both patient:clinician relationships and rapport between coworkers. (I’d love to talk about healing environments another time.)
With that said, here are some practical tactics that seem to generate meaningful results:
1. Set clear, accurate expectations.
Primary outcomes: reduced anxiety; improved rapport; patient/caregiver empowerment.
From prognostication to unexpected delays, people benefit tremendously from knowing what to expect. In hospice, it’s vital to use plain language to talk about disease progression. When caregivers understand where their loved one is headed, they can logistically and emotionally prepare for the future. They can also feel more confident and comfortable providing care.
There’s a lot of data about how perception of clinician efficacy and quality diminish the longer a patient waits to see their provider. Since it can be difficult to change clinician behavior, a simple way to sway opinion is to graciously keep people informed about delays. (In one survey, 80% of the 5,000 respondents said learning the wait time would minimize or completely eliminate their frustration.)
With so much uncertainty in our lives, speaking clearly, honestly and early about health and wellbeing is fundamental to true quality and compassionate care.
2. Strive to be fully present.
Primary outcomes: heightened quality; patient-centered care; enhanced experience of work; increased trust and rapport.
Research (and common sense) demonstrate the importance of constructive communication in healthcare. Listening may be the most essential gift a clinician can offer. It requires slowing down, setting aside agendas, and honing our senses.
I know a physician acupuncturist who uses 4-5 rooms simultaneously, each space occupied by a seemingly endless rotation of patients over the course of a day. He flashes from room to room like a hummingbird, rarely spending more than 10 minutes in one place. Still, when he is with his patients, his attention is wholly on them – they feel connected and heard. Through his non-judgmental presence, he opens a window to collaborative inquiry and exploration. And, though their time together is limited and interrupted, he has remarkably high patient satisfaction scores. Yes, he’s an excellent doctor, and he’s also a deeply present listener committed to patient-centered care.
Most healthcare environments are wildly hectic and we tell ourselves all kinds of scarcity stories about time... annnnd we can only serve one person in a given moment. Learning to slow down and focus takes practice; luckily, there are endless ways to develop this kind of healing presence. There’s a ton of research on mindfulness in particular, and healthcare-specific trainings in it, too.
3. Nurture compassion in the workplace.
Primary outcomes: improved rapport; increased workplace joy; heightened sense of community.
A beloved mentor has a great mantra: “Every encounter can be a healing encounter.” As a healthcare administrator, she believes she contributes directly to patient care through thoughtful, engaging interactions with people in Finance, HR and throughout the organization. She trusts that warmth and compassion soften the mind, ease the heart, build community and can have vast downstream influence. This pay-it-forward mindset acknowledges our humanity and liberates us from stiff communication styles, without compromising professional boundaries.
We expect clinicians to extend kind-hearted respect to their patients, so I’m always baffled when colleagues don’t do the same for one other. This may be viewed as an acceptable byproduct of a busy, demanding environment, however: what we permit, we promote. Further, this conduct diminishes trust, safety and respect, for patients and the entire team. Bringing a compassionate spirit to colleagues can be profound medicine, one that generates wholeness and joy, and fosters our ability to serve others.
4. Cultivate a culture of gratitude.
Primary outcomes: improved patient perception of care; workplace joy; employee satisfaction and retention.
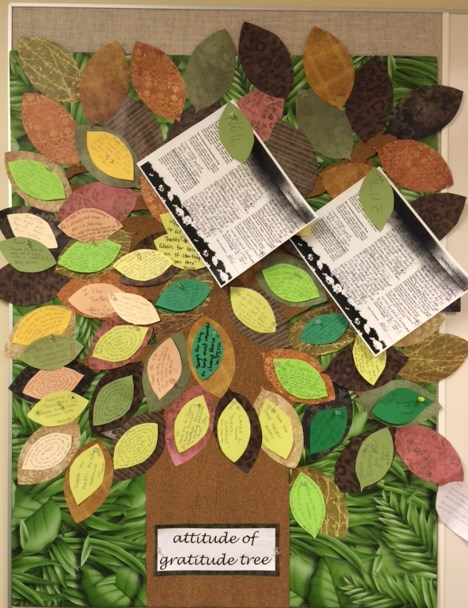 It can be painful (yes, painful) to work in healthcare if your priority is high quality service. To offset all the rules and regulations, complaints and missteps, acknowledging what’s working well and extending praise truly enlivens the spirit. Gratitude keeps people rooted in their abundance, improves self-care and resiliency, and strengthens relationships – all indispensable attributes for care providers. (Here’s a video that takes the topic deeper.)
It can be painful (yes, painful) to work in healthcare if your priority is high quality service. To offset all the rules and regulations, complaints and missteps, acknowledging what’s working well and extending praise truly enlivens the spirit. Gratitude keeps people rooted in their abundance, improves self-care and resiliency, and strengthens relationships – all indispensable attributes for care providers. (Here’s a video that takes the topic deeper.)
Another benefit of praise – the more you recognize a person’s good deeds, the easier it is to come forward when something isn’t working. They already feel seen and valued, which may enable them to readily trust your perspective.
I’m a fan of both private and public praise, and I aim to be as specific as possible. Descriptive praise feels good and reinforces what’s most important.
Posted by Jodi Fishkin Manning on Nov 5, 2018
SHARE YOUR REFLECTION
4 Past Reflections


On May 31, 2023 BryanDum wrote:

On May 31, 2023 Wesleyset wrote:



On May 31, 2023 MarcusTwipT wrote:
Post Your Reply